Thyroid Cancer
Thyroid Cancer by Terry Ryan Surprisingly, I have had 2 friends diagnosed with thyroid cancer this last month. Both are female and in their 50s. So, and of course, I had to research THYROID CANCER to find out what it is and what to do. Thyroid cancer has doubled since the 70s. It is fifth […]
Cure Cancer With The Hallelujah Diet? by Terry Ryan

[hupso] Cure Cancer With The Hallelujah Diet? by Terry Ryan My neighbor claims the Hallelujah Diet saved her uncle who had cancer of the eye, and that’s how I first heard about the mysterious diet. Hmmm, a diet that saved a person from cancer. I had to learn more. Googling the Hallelujah Diet, I found […]
Pancreatitis!
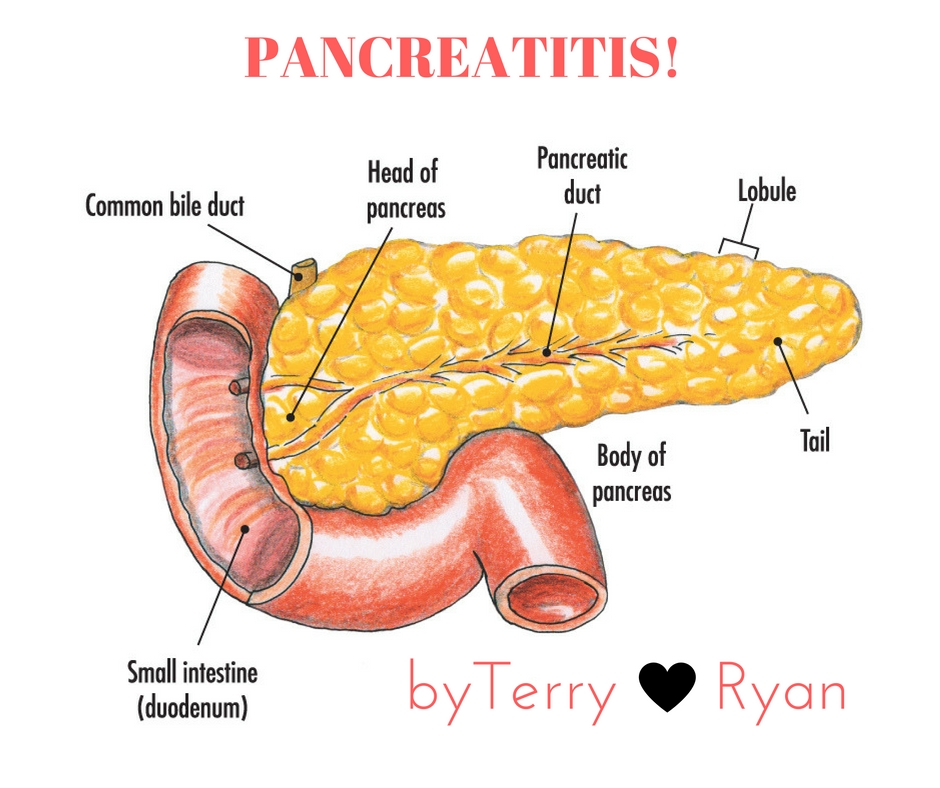
I was inspired to write this post, sadly, because I have a neighbor that I will call, Annie,who is suffering with pancreatitis. What is pancreatitis? It is inflammation of the pancreas, according to MedicineNet.com. This typically happens when the digestive enzymes found inside the pancreas become active, causing inflammation and even damage to the organ. Annie […]
DCIS — Ductal Carcinoma In Situ and What to Do?
Well, they did it again. After years of scaring the daylight out of women—basically making women fear their own breast, the medical community changed another directive, this time about Ductal Carcinoma In Situ, DCIS. In the news for the last couple of days is this heading for example: Doubt Is Raised Over Value of Surgery […]
Turmeric-The Spice For a Longer and Healthier Life

Turmeric is a common spice, you may already have in your cupboard, that may be used for improved health. The spice has been said to: Prevent heart disease Stave off Alzheimer’s disease Eliminate depression Alleviate joint pain…and more How does this work? Inside turmeric is a compound called curcumin which is responsible for the orange […]