Health
now browsing by category
What Killed Bill Paxton?
What killed Bill Paxton by Terry Ryan
Bill Paxton, 61, actor, father, and husband, passed away Saturday, February 25, 2017 due to complications from surgery. He underwent heart surgery and suffered a stroke afterwards. (Source: TMZ)
Potential Complications During and After Heart Surgery
Some of the more common complications of heart surgery are routinely dealt with during the hours and days of recovery in the hospital. The patient is closely monitored for these complications by staff.
- Bleeding: May occur at the incision site or from the area of the heart where surgery is performed
- Abnormal heart rhythm: In rare cases a temporary external, or permanent internal pacemaker may be necessary to correct this problem.
- Ischemic heart damage: Damage to heart tissue caused by a lack of blood flow to the heart
- Death: The risk of death is increased in surgeries where the heart is stopped for the procedure.
- Blood clots: Clots may form in and around the heart or travel through the bloodstream.
- Stroke: Often caused by clots that form in the blood after surgery
- Blood Loss: In some cases, a transfusion may be necessary.
- Emergency surgery: If a problem is discovered after surgery, an emergency surgery may be necessary to repair any problems.
- Cardiac tamponade (pericardial tamponade): A life-threatening condition where the pericardium, the sac surrounding the heart, fills with blood. This makes it difficult, or impossible, for the heart to fully function. (Source: https://www.verywell.com/heart-surgery-complications-and-risks-3156953)
Other side-effects include heart attack, respiratory complications, bleeding complications, infections, high blood pressure and stroke. When the vessels around the heart are clamped shut during the operation, plaque breaks off of the inner walls. Blood then carries this debris to the brain, where it causes numerous “mini” strokes.
About 70-80% of patients undergo bypass surgery remain free of chest pain (angina) for one year. But this doesn’t last forever. Within three years of the operation, up to one-third of patients will suffer from chest pain again.
Long-term studies indicate that only certain subsets of heart disease patients live longer because of their bypass operation.
What to do? A vegetarian diet could prevent and even reverse heart disease.
If all the parts of your circulatory system—the veins, arteries and capillaries—were placed end to end, they would stretch for more than 60,000 miles. That’s more than two times around the earth! But one tiny blockage could bring all 60,000 miles to a halt. Doctors use many medicines and surgical procedures to keep the system running.
But back in 1990, a major shift began in medical practice. That was the year that a young doctor in California published a study that set out to test whether heart disease could not simply be prevented, but might actually be reversed. And he wanted to see if it could be done, not with surgery or drugs, but with diet and lifestyle changes alone.1 This notion was inconceivable to some. After all, heart disease was a one-way street unless it was treated with cholesterol-lowering drugs, heart pills, and when needed, open-heart surgery.
Dr. Dean Ornish, a Harvard-trained physician, studied 47 patients in the San Francisco Bay Area, all of whom had significant heart disease. That is, the coronary arteries that brought blood and oxygen to their hearts were starting to narrow, pinching off blood flow and threatening the viability of the heart. Some had already had heart attacks. He assigned half of the patients to a control group that received the standard care that doctors usually prescribe, meaning a diet centered on “lean” meat, poultry, and fish, along with various medications and the usual advice not to smoke.
The remaining patients were assigned to a very different program. They were asked to follow four steps:
- A low-fat, vegetarian diet
- Brisk walking for a half-hour per day or an hour three times per week
- No smoking
- Stress management exercises
He used a vegetarian diet, because cholesterol and saturated fat are found mainly in animal products. So the prescribed diet excluded red meat, poultry, and fish, virtually eliminating cholesterol and animal fat. It reduced all sources of fat, including vegetable oils. But Dr. Ornish used no drugs at all—not even cholesterol-lowering drugs. The program consisted only of simple diet and lifestyle changes.
One year later, all patients had an angiogram—a special x-ray that reveals the blockages in the coronary arteries, and the results were compared to the same sort of test done at the beginning of the study. The results made medical history. The control-group patients, who had been following the more traditional medical routine, had not generally improved. In fact, the blockages in their coronary arteries were worse, on average, than at the beginning of the study. They still had chest pain and still needed medications. That was not news. Despite typical heart treatments, heart disease usually worsens as time goes on.
For the patients in the experimental group, however, the story was very different. Chest pain began to disappear within weeks. Their cholesterol levels dropped dramatically. And their coronary arteries, which had been gradually closing off, year after year, were actually starting to reopen. In fact, the effect was so great that angiograms showed clear evidence of reopening in 80% of patients in the first year.
These results were published in The Lancet in 1990 and gave doctors a new tool for reversing heart disease. The program cost much less than surgery, was surprisingly easy to follow, and could help keep patients healthy over the long run. The only “side effects” were good ones: the average patient lost 22 pounds in the first year!
A Cleveland Clinic surgeon, named Caldwell Esselstyn, used the same type of diet for severely ill heart patients.Some of the patients had been told they had less than a year to live. But of the 17 patients who stuck to the program, there was not a single cardiac event over the next 12 years! They were alive and well—and had reversed their disease. (source: https://www.pcrm.org/about/volunteer/preventing-and-reversing-heart-disease)
The Bill Clinton Diet
When President Bill Clinton suffered from debilitating chest pain, he was living on the typical American diet of meat and potatoes.
In the White House, Bill Clinton’s appetite was legend. He loved hamburgers, steaks, chicken enchiladas, barbecue and french fries but wasn’t too picky. At one campaign stop in New Hampshire, he reportedly bought a dozen doughnuts and was working his way through the box until an aide stopped him.
Former President Clinton now considers himself a vegan. He’s dropped more than 20 pounds, and he says he’s healthier than ever. His dramatic dietary transformation took almost two decades and came about only after a pair of heart procedures and some advice from a trusted doctor. (Source: http://www.cnn.com/2011/HEALTH/08/18/bill.clinton.diet.vegan/)
Instead of people waiting for heart disease to stop them in their tracks, start adopting a vegetarian diet. Not only will your heart “thank you,” but so will your eyes, your skin, your everything. Your life.
Conventional medicine is great! You have a broken leg, infected toe, sore throat, etc. they are there for you and can help you heal. But they can’t do all the work. It is up to you to take the mature steps to a healthy and long life. That means taking care of yourself, unless you want to someday lay on a table in an operating room counting down from 100 for the anesthesia to kick in. As we all know from what happened to Bill Paxton, that outcome is not always in your favor.
Things to stop right now for a better life:
- Give up smoking (Are you kidding? You are still smoking?)
- Alcohol…nope
- White sugar – the devils poison. Stop eating sugar
- Eating things like prime rib. Come on! Self-explanatory
- Not taking time to smell the roses. Stress is a killer!
- Illegal drugs (Bad idea)
I’d like to add that Bill Paxton was one of my favorite actors, and I am so sorry for his family’s loss. What a tragedy and was it possibly preventable with a vegetarian diet. That question will never be answered. He could have had a family history of heart disease and genetics played a big part in this equation.
My suggestion is put the odds in your favor. People depend on you and you deserve a healthy and happy life. Eat more vegetables!
Thanks for reading!
 Terry Ryan, Health Blogger
Terry Ryan, Health Blogger
Pancreatitis!
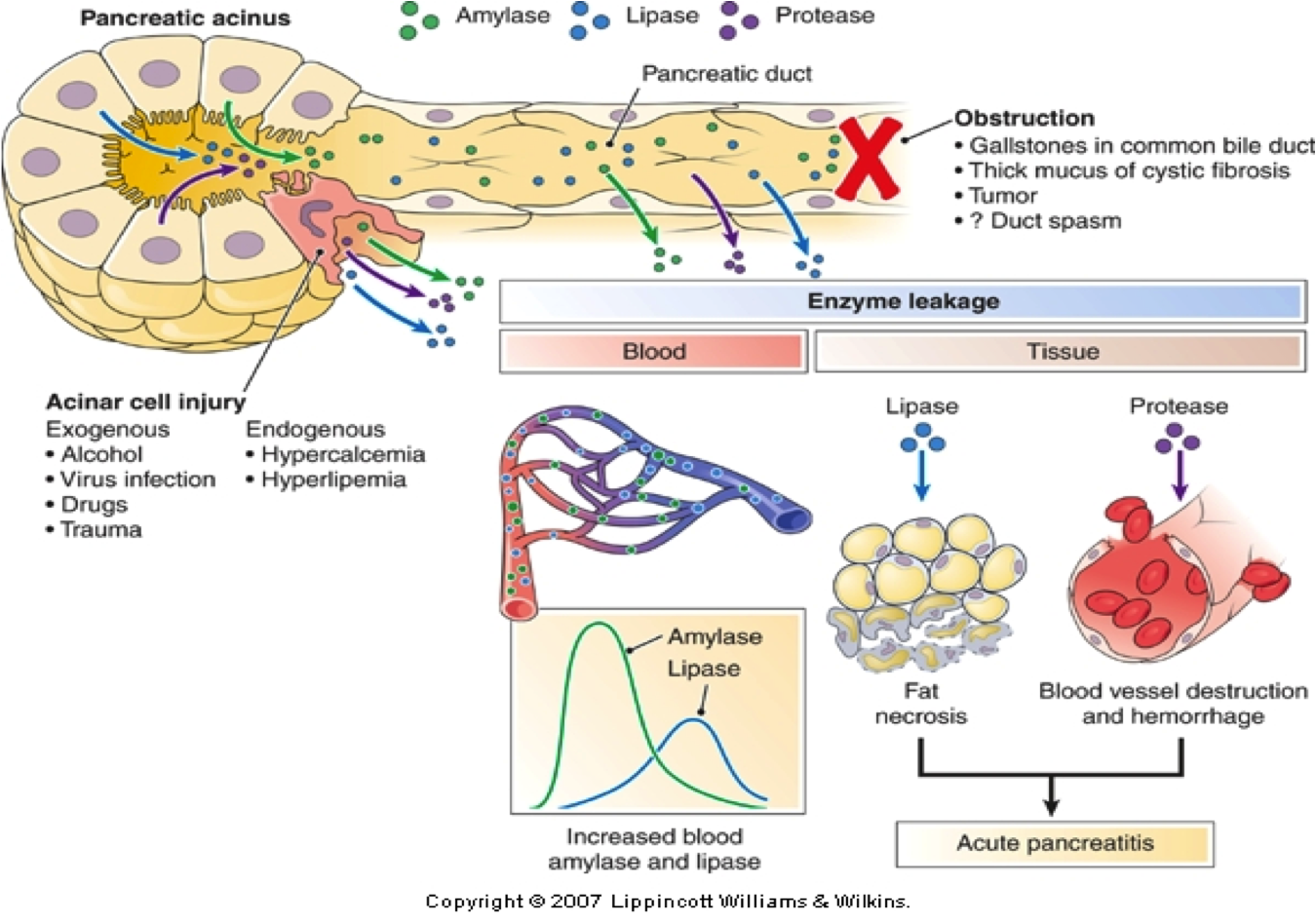
I was inspired to write this post, sadly, because I have a neighbor that I will call, Annie,who  is suffering with pancreatitis. What is pancreatitis? It is inflammation of the pancreas, according to MedicineNet.com. This typically happens when the digestive enzymes found inside the pancreas become active, causing inflammation and even damage to the organ.
is suffering with pancreatitis. What is pancreatitis? It is inflammation of the pancreas, according to MedicineNet.com. This typically happens when the digestive enzymes found inside the pancreas become active, causing inflammation and even damage to the organ.
Annie has had a lot of pain in her left side that would radiate to her left shoulder. She also is constantly nauseated and these painful attacks would come on without warning. Surprisingly, it took a long time and several attacks, plus doctor visits and trips to the emergency room, for Annie to 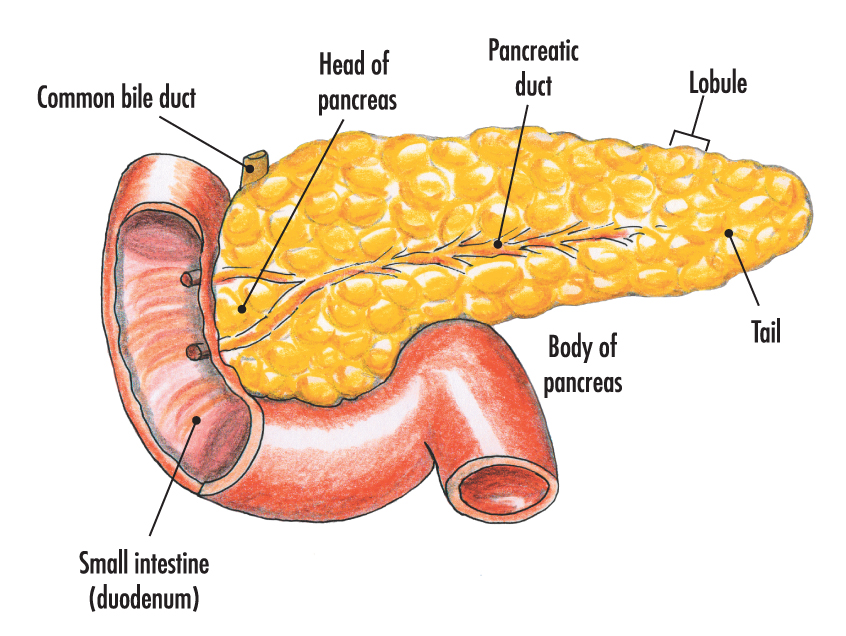 be diagnosed. Annie’s husband and I Googled her symptoms and came up with our amateur diagnoses prior to the doctors confirming it was indeed pancreatitis. Believe me when I say, we did not want to be right.
be diagnosed. Annie’s husband and I Googled her symptoms and came up with our amateur diagnoses prior to the doctors confirming it was indeed pancreatitis. Believe me when I say, we did not want to be right.
Pancreatitis can either be acute or chronic, as stated by MedicineNet.com. Acute, or sudden, pancreatitis is sometimes caused by the presence of gallstones, which are small, pebble-like masses of hardened bile that form in the gallbladder and can cause irritation when they pass through the common bile duct. Heavy alcohol use is another common cause of acute pancreatitis.
Most cases of chronic, or long-term, pancreatitis are caused by long-term alcohol abuse, cystic fibrosis or hereditary disorders, according to WebMD. In about 25 percent of cases, the causes of chronic pancreatitis are unknown.
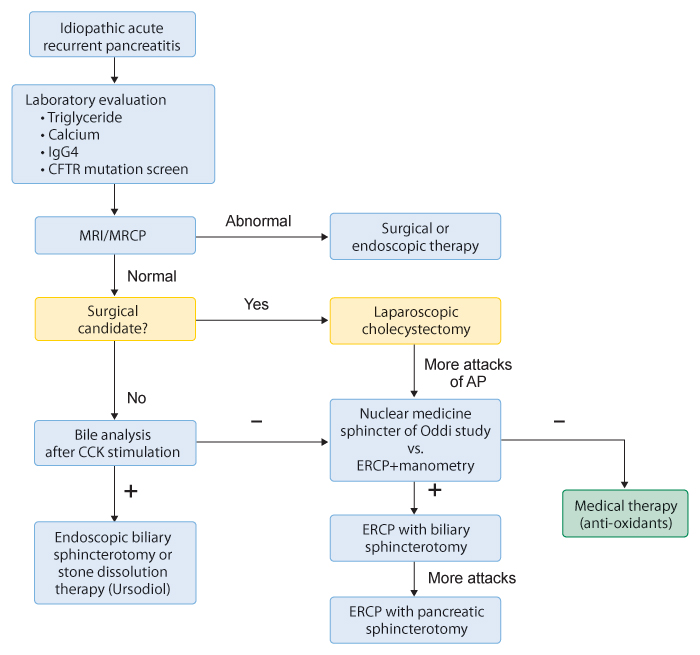
Annie was first rushed to the ER the day after Thanksgiving 2015, and she continues to suffer with the debilitating symptoms. Today’s date is 12/15/2016. Medical intervention has done little to relieve the recurring attacks. She has lost around 30 pounds and is scared to eat fearing that it may bring on an attack. A few weeks ago, she had an outpatient procedure when a stent was inserted into a duct in her pancreas that helps fluid drain into her stomach and hopefully eliminating the attacks. Yesterday, she was experiencing more pain so the stent was not a successful procedure.
What is the pancreas?
The pancreas is a small organ located behind the stomach in the abdomen (the size of a dollar) and functions as a digestive organ and an endocrine organ. In the digestive system, the pancreas helps break down food. In the endocrine system, the pancreas releases key hormones, such as insulin and glucagon.
What is Chronic Pancreatitis?
Chronic pancreatitis is inflammation of the pancreas that does not heal or improve—it gets worse over time and leads to permanent damage. Chronic pancreatitis eventually impairs a patient’s ability to digest food and make pancreatic hormones. Industrialized countries have estimated an annual incidence rate of 5-12/100,000 people who will develop chronic pancreatitis. The prevalence of chronic pancreatitis is 50/100,000 people. Chronic pancreatitis often develops in patients between the ages of 30 and 40, and is more common in men than women.
What blood test are preformed at the ER?
To confirm whether a person has pancreatitis Blood tests can evaluate the function of the gallbladder, liver, and pancreas. Levels of the pancreatic enzymes amylase and lipase can be measured. Blood tests can also check for signs of related conditions, including infection, anemia (low blood count), and dehydration. A tumor marker called CA 19-9 may be checked if pancreatic cancer is suspected.
Here is a scenario:
A person arrives at the ER complaining of intense pain in their left quadrant along with nausea. The P.A. or the nurse who first evaluates the patient will use this mnemonic tool: OPQRST
O = Onset – The word “onset” should trigger questions regarding what the patient was doing just prior to and during the onset of the specific symptom(s) or chief complaint. • What were you doing when the symptoms started? • Was the onset sudden or gradual? It may be helpful to know if the patient was at rest when the symptoms began or if they were involved in some form of activity. This is especially true with patients presenting with suspected cardiac signs & symptoms.
P = Provoke – The word “provoke” should trigger questions regarding what makes the symptoms better or worse. • Does anything you do make the symptoms better or relieve them in any way? • Does anything you do make the symptoms worse in any way? This is sometimes helpful in ruling in or out a possible musculoskeletal cause. A patient with a broken rib or pulled muscle will most likely have pain that is easily provoked by palpation and/or movement. This is often in contrast to the patient having chest pain of a cardiac origin whose pain is not made any better or worse with movement or palpation.
Q = Quality – The word “quality” should trigger questions regarding the character of the symptoms and how they feel to the patient. • Can you describe the symptom (pain/discomfort) that you are having right now? • What does if feel like? • Is it sharp or dull? • Is it steady or does it come and go? • Has it changed since it began?
R = Region/Radiate – The words “region and radiate” should trigger questions regarding the exact location of the symptoms. • Can you point with one finger where it hurts the most? • Does the pain radiate or move anywhere else? Although it is not always easy for a patient to identify the exact point of pain, especially with pediatric patients, it is important to ask. Asking if they can point with one finger to where it hurts the most is a good start. From there you will want to know if the pain “moves” or “radiates” anywhere from the point of origin.
S = Severity – The word “severity” should trigger questions relating to the severity of the symptoms. • On a scale of 1 to 10, how would you rate your level of discomfort right now? set.
T = Time – The word “time” should trigger questions relating to the when the symptoms began. • When did the symptoms first begin? • Have you ever experienced these symptoms before? If so, when?
Next blood tests, abdominal X-rays,EKG, blood pressure, oxygen saturation tests will be administered along with a stethoscope placed on the patient’s abdomen to listen for intestinal sounds. If a patient is experiencing a pancreatic attack then the intestines will be quiet.
Pain medicine will be administered and usual the patient will be admitted and placed on IV to keep them hydrated and a strict no food protocol will be prescribed for a few days until the pain subsides.
The Pancreatitis Diet
Pancreatitis patients require varying amounts of fat, depending on factors such as weight and height; however, for most patients, the recommended limit is 20 grams of fat per day, states the National Pancreas Foundation. Each meal should not exceed 10 grams of fat content. A carrot and sweet potato soup with cranberry relish and a blend of black beans, carrots, lime juice and red peppers are healthy appetizers. Citrus chicken with cumin and oregano makes a great main dish.
For patients who suffer a flare, doctors typically suggest avoiding solid foods for one or two days, notes the National Pancreas Foundation. Severe pain requires patients to start a diet of clear liquids. Because this type of diet lacks nutrition, patients should gradually add other food items based on the instruction of their doctors.
It is crucial for pancreatitis patients to avoid drinking alcohol, as alcohol consumption can cause pancreas to flare due to dehydration, explains the National Pancreas Foundation. To keep the body properly hydrated, physicians often recommend carrying a bottle of water at all times.
Do’s and Do Not’s for Acute Pancreatitis Diets
 Do’s
Do’s
- Eat snacks throughout the day rather than large meals
- Eat foods low in fat (a max of 30 grams of fat a day)
- Eat foods high in “lean” protein like beans, chicken, fish, lean cut beef, etc…
- Eat foods that are high in antioxidants like berries, oranges, and broccoli
- Eat foods that have good amounts of vitamins C, B9, and B12
- When you do eat fat, pick foods high in Omega-3 fatty acids like Salmon, flaxseed, walnuts, etc…
- Try and drink anywhere from 6-8 glasses of water daily
Do Not’s
 Stay away from spicy foods of any type
Stay away from spicy foods of any type- Try and rid yourself of caffeine, cigarettes, and alcohol
- Limit foods that stimulate the gut such as peppermint and black pepper
- Diminish your sugar intake as much as possible (sugar causes inflammation)
- Limit your use of foods like butter, bacon, margarine, etc..
- Use fat-free (or low fat) dressings with the idea that less is better
- Get rid of processed grains like white bread, and say hello to 100% whole grain
- Don’t touch fried foods
If you want to avoid acute pancreatitis and of course, chronic pancreatitis, there are a few things you will need to keep in mind.
Fats and processed foods are some of your biggest enemies. The typical modern diet makes these foods difficult to avoid. You want to keep your pancreas from being overloaded. So eating small portions and avoiding foods that stress your pancreas is important. Some experts recommend eating six small meals a day with a supplement of pancreatic enzymes each time.
Processed and fatty foods are literally everywhere. Try to stick with fresh foods as much as possible. Avoid frozen meals and canned meals. Avoid boxed foods like cold cereal and crackers.
Basically, if it can sit on your shelf and not go bad for months and months, you may want to think twice about eating it.
Avoid drinking alcohol and smoking as well. These two activities can make your pain worse and increase your risks.
Ideas for Breakfast, Lunch, and Dinner
Acute pancreatitis diets can be difficult to find. Although there are many limitations to what you should and shouldn’t eat, you can still enjoy food and put together great meals. One thing to keep in mind when doing so is to try and stick to a fairly routine schedule, also providing assistance in providing some relief to the workload of your pancreas. Below are some ideas for putting meals together to form a complete and good Acute Pancreatitis Diet plan for you. As you try these combinations see what works for you and stick to those foods that do.
[yikes-mailchimp form=”1″ submit=”Click Here”]
Breakfast
- Yogurt w/ granola
- Oatmeal
- Egg Whites w/ tomato
- Wholegrain cereal w/ banana
Lunch
- Chicken w/ brown rice and broccoli
- Tuna sandwich w/ vegetable soup
- Whole wheat pasta w/ asparagus
Dinner
- Salmon w/ spinach
- Lean meat w/ sweet potatoes
- Chicken Salad w/lite dressing
The Big Question….Will Pancreatitis turn into Pancreatic CANCER?
There is a connection from acute to chronic pancreatitis and from chronic pancreatitis in time to cancer of the pancreas. The Internet says studies have shown that congenital conditions with chronic pancreatitis have a higher incidence of cancer of the pancreas later in life. The tumor markers should be checked from time to time in these high risk patients. Also the physician will likely order CT scan studies more often in these patients to monitor for any transition towards a cancerous degeneration.
In Conclusion…
Take special care of your pancreatitis when you start having attacks. Eat a low fat diet and stay away from junk food, alcohol and cigarettes. Find a great medical support team that specializes in Pancreatitis and follow Pancreatitis Facebook groups.
More resources:
Thank you for reading,
Terry Ryan, Health Blogger
Vague about the Vagus Nerve?

Vague about the vagus nerve? Don’t feel alone because most people are. Did you know it is referred to by the medical community as the MIRACLE NERVE?
>>>>>Read this story about a Super Woman! Wow! Things you find on the web!<<<<<<
I first became aware of the importance of the vagus nerve while watching a medical mystery show on TV. The main character in the true story, a woman, kept on passing out while she was eating. The doctors were stymied and she bounced to specialist after specialist until one finally diagnosed her with a vagus nerve abnormality. Every time she ate something the food would apply pressure to her vagus nerve and she would pass out. Weird and very unusual but it peaked my interest.
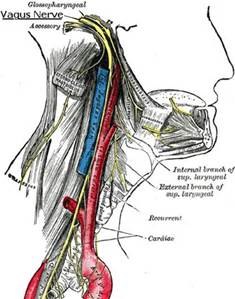
What is a vagus nerve? The vagus nerve is either one of two cranial nerves which are extremely long, extending from the brain stem all the way to the viscera. The vagus nerves carry a wide assortment of signals to and from the brain, and they are responsible for a number of instinctive responses in the body. (The vagus nerves are paired; however, they are normally referred to in the singular.)
The vagus nerve helps to regulate the heart beat, control muscle movement, keep a person breathing, and to transmit a variety of chemicals through the body. It is also responsible for keeping the digestive tract in working order, contracting the muscles of the stomach and intestines to help process food, and sending back information about what is being digested and what the body is getting out of it.
When the vagus nerve is stimulated, the response is often a reduction in heart-rate or breathing. In some cases, excessive stimulation can cause someone to have what is known as a vaso-vagal response, appearing to fall into a faint or coma because his or her heart rate and blood pressure drop so much. Selective stimulation of this nerve is also used in some medical treatment; vagus stimulation appears to benefit people who suffer from depression, for example, and it is also sometimes used to treat epilepsy.
Most of the time, you don’t notice the actions of the right and left vagus nerves, but you probably would notice if this nerve ceased to function as a result of disease or trauma, because the vagus nerve is one of the many vital nerves which keeps your body in working order. Without the functions of the vagus nerve, you would find it difficult to speak, breathe, or eat, and your heartbeat would become extremely irregular.
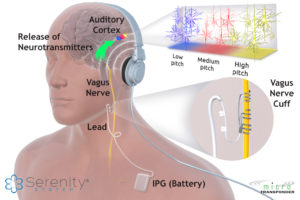
Vagus nerve stimulation has been used to treat obesity, tinnitus, Crohn’s disease, strokes and headaches. Vagus nerve stimulation is going to be used more and more in the future.
The Treatment
Gentle pulses of electricity is applied to the vagus nerve. It is relatively painless. The FDA has approved an device that is implanted in the neck and connected to the vagus nerve to treat obesity. The vagus nerve is full of fibers like an electric wire, and each wire relates to a different area in your body. It turns out that the vagus nerve tells your stomach when to empty and your brain when it is full.
How to self-stimulate your vagus nerve
 chest cavity and stomach cavity. Also known as “belly breathing,” diaphragmatic breathing is characterized by an expansion of the abdomen instead of the chest.
chest cavity and stomach cavity. Also known as “belly breathing,” diaphragmatic breathing is characterized by an expansion of the abdomen instead of the chest.Read more: Simple Trick to Relieve Stress: Vagus Nerve Stimulation
My husband purchased a device that helps him slow his breathing in an attempt to naturally lower his stress and blood pressure. He lies in bed with ear phone on and tries to breath along with the tempo of the machine. I have tried it and it was really difficult to slow my breathing to the timing of the machine, but according to my husband, it works.
Here is his Resperate

In the future researchers will find ways to harness the power of the vagus nerve from outside the body through the ear, skin or devices delievered by needles or just a topical ointment.
The human body is amazing. Thank you for reading my blog on the vagus nerve.
Be healthy,

Terry and Lucky
Terry Ryan, Blogger
How Well Your Balance is Indicates Health

 Did you know that how well you can balance on one leg is a good indicator of your physical and metal health? The older you are the more likely you will have issues with your balance.
Did you know that how well you can balance on one leg is a good indicator of your physical and metal health? The older you are the more likely you will have issues with your balance.
When a toddler or child falls, he or she usually shakes it off and keeps moving. But when an older adult falls, there are often consequences. Broken bones limit mobility. They can also lead to a downward health spiral. Each year, thousands of older Americans die as a result of breaking a hip. Broken bones and head injuries can knock confidence, create a fear of falling, and undermine independence.
As we age
As we age, cells in the vestibular system die off,
A number of changes that come with aging can affect our balance.
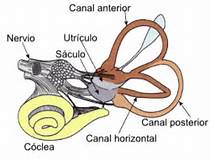
- Inside our ears is a balance center called the vestibular system that detects where our body is in space. Are we upright or lying flat; are we standing on our feet or performing a handstand?
The vestibular system is connected to centers in the brain that also control our balance. When the vestibular system and brain determine that we’re about to fall over, the brain directs the body to take corrective action. Maybe we twist back upright so we don’t fall. Maybe we’re too far off center to avoid falling, so our arms and hands stretch out to brace our fall.As we age, cells in the vestibular system die off. This affects how accurately we detect our position in space. That, in turn, affects our ability to correct our position. For example, if we
 start to tilt to the right and the vestibular system doesn’t detect this quickly, it becomes harder for the brain to prevent falling to the right.
start to tilt to the right and the vestibular system doesn’t detect this quickly, it becomes harder for the brain to prevent falling to the right. - Our sight, the ability to focus and see things clearly, diminishes with age. So do depth perception, night vision and sensitivity to contrast. Eye problems can impair, blur or distort vision. The loss of these visual cues compromises balance. Corrective lenses or surgery may help.
- Blood pressure can dip suddenly when you stand up, causing dizziness, lightheadedness, blurry vision, even fainting. Standing up slowly — sitting first on the side of the bed when you rise, for example — may help.
- We lose a lot of muscle mass and strength as we age. We also lose power — a function of strength and speed — which affects balance, too. If you start to trip, power helps you react swiftly. Exercise can help you rebuild strength and power, or at least slow the pace of decline.
- Our reflexes and coordination slow with age. Thus, you may be more likely to stumble — and take more time to react when you do.
An Amazing 100% Scientific Research-Based Method 
Treats Root Cause of Dizziness and Other Balance
Problems in As Little As 14 Days* ! CLICK HERE
Many health problems can interfere with balance. They include, but are not limited to, arthritis, stroke, Parkinson’s disease and multiple sclerosis.
Medications may also increase your risk of falls. They can cause blurred vision, dizziness, lightheadedness and drowsiness. Some medications may damage the inner ear, spurring balance disorders.
Along with regular aerobic exercise and weight training, balance exercises are important as we get older. Such exercises really can help you improve your balance. (Source: http://www.askdoctork.com/why-does-balance-decline-with-age-201306054928)
I’ve noticed a balancing problem with my then 79 year-old mother. One day we were walking and I witnessed her doing the “old-person shuffle.”
Become a Certified Self-Esteem Coach for Children and Learn the Life-Impacting Secrets to Champion Kids to Elevate their Self-Esteem & Live their Best Lives
“Why are you walking like that?” I said horrified to see my mother actually show signs of aging.
“My brain isn’t communicating with my feet,” said my mother.
I never thought my mother would have a problem with her walking or balance. She was a person who was more comfortable walking in the woods picking mushrooms than she was shopping in a mall. Mystified that she said her brain wasn’t communicating to her feet I decided to research and see if there was a way to improve my mother’s balance. While staying active physically at any age it is also important to keep the mind active. I’ve noticed people who retire suddenly decline physically and mentally in the supposed “Golden Years.” And I’ve seen active seniors in their 80s playing pickleball against people in their 60s; the 80+ year-olds just as fast moving and quick thinking as the 60 year olds.
Balance Board provides great balancing exercises(Click here)
- Improves core strength, functionality, sense of balance, visual sense
- Helps to strengthen the targeted muscles, ligaments, tendons and joints
- Relax the muscles and release your stress away and enhance self confidence
- Great for rehabilitation centers, gyms, professional athletes and individual
 In my observations, seniors that take care of their health or more likely to maintain good balance. They eat well, limit their alcohol, skip the sugary snacks and will walk or engage in other physical activities.
In my observations, seniors that take care of their health or more likely to maintain good balance. They eat well, limit their alcohol, skip the sugary snacks and will walk or engage in other physical activities.
The above activities also provide social connections; very important for mental health in seniors.
Some basic balance exercises you can do anytime include:
- One-legged stands: Stand on one foot for 30 seconds, or longer, then switch to the other foot. You can do this while brushing your teeth or waiting around somewhere. In the beginning, you might want to have a wall or chair to hold on to.
- Heel rises: While standing, rise up on your toes as far as you can. Then drop back to the starting position and repeat the process 10 to 20 times. You can make this more difficult by holding light hand weights.
- Heel-toe walk: Take 20 steps while looking straight ahead. Think of a field sobriety test.
- Sit-to-stand: Without using your hands, get up from a straight-backed chair and sit back down 10 to 20 times. This improves balance and leg strength.
 Just as the body needs physical exercise to keep fit, the brain needs mental exercise to stay active and alive. Mental exercise stimulates the brain, often providing long-lasting positive effects regarding thinking and reasoning skills, memory and processing speed.
Just as the body needs physical exercise to keep fit, the brain needs mental exercise to stay active and alive. Mental exercise stimulates the brain, often providing long-lasting positive effects regarding thinking and reasoning skills, memory and processing speed.
Playing games such as cards, mah jong, and hobbies are a great way to keep a senior’s mind sharp.
Depending on the seniors interests and abilities, the following are examples of possible crafts or hobbies they may enjoy.
- Drawing
- Painting
- Knitting
- Playing music
- Scrapbooking
- Woodworking
- Mosaics using tiles or colored paper
- Photography
Keeping the mind active and constantly learning and stimulating the brain will help with balance.
Don’t just age, but improve with age!
Thanks for reading!
Terry Ryan, Blogger













 D5 Creation
D5 Creation